CDC guidelines protect staff, medical personnel, visitors & patients
One of the best ways to protect against the COVID-19 is to avoid contact with the virus. Do not touch it. Do not breathe it. Maintain six feet of distance between people. Use the prescribed personal protective equipment (PPE).
COVID-19 is an equal opportunity virus. It threatens everyone without regard for age, sex, or socio-economic status. It affects leaders of countries, doctors, nurses, and incarcerated individuals equally. It has no respect for the economy or business timelines. As Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, says, COVID-19 has its own timeline.
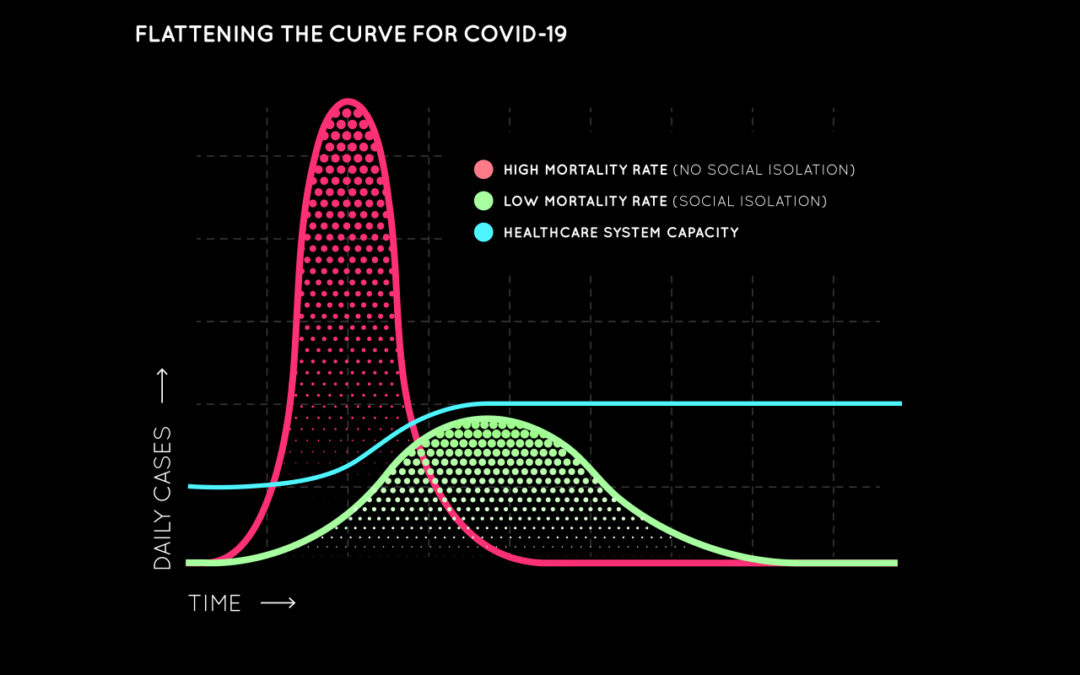
The best advice for avoiding COVID-19 is to minimize contact to the virus by distancing oneself from others – even those who look healthy. Sounds good, except to those who work and live in a detention setting, where social distancing can be challenging. What can you do to flatten the curve? Prepare, prevent, and manage the spread of the virus.
The U.S. Centers for Disease Control and Prevention (CDC) last week released its Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities. This guide, written for all custodial, civil, and pre-trial detention settings, provides guidance on how to prepare, prevent, and manage the spread of the virus with hands-on explanations.
During last week’s video conference with partners, Wellpath Chief Clinical Officer Tom Pangburn, MD, and Associate Chief Clinical Officer William Ruby, MD, told participants that Wellpath will follow the CDC guidelines and urged them to follow its guidance. The CDC provides ways to recognize and minimize contact with the virus, how to implement social distancing, and how to deal with staff fluctuations. Following are a few examples:
- Keep the virus from coming in. We enforce pre-intake screening and temperature checks for all entrants in the sally port before intake. If COVID-19 is expected (fever, cough, shortness of breath), we will provide the patient a facemask and isolate him/her as appropriate. Small facilities without adequate isolation areas contact the local health department for guidance. We quarantine and monitor suspected cases for 14 days. Our staff uses face masks and other PPE based on CDC criteria and best practices. Wellpath’s procurement organization will continue to secure needed equipment, but the nation’s PPE supplies are severely strained. When you have access to additional supplies through state and federal agencies, we encourage your assistance in obtaining PPE, medical supplies and test kits to help us all meet this challenge.
- Implement social distance. Where possible, implement strategies to increase the space between individuals by at least six feet. That can be as simple as removing every other seat in a waiting room, staggering time in recreation spaces, staggering meals or serving meals in cells, limiting group activities, and arranging bunks head-to-foot to put distance between heads. Consider telehealth to protect care givers and patients. Wellpath conducts more than 100,000 telehealth encounters each year. We expect that number to increase dramatically. During the pandemic, Health and Human Services (HHS) will waive potential penalties for HIPAA violations against healthcare providers using everyday communications technologies. This applies to widely available communications apps, such as FaceTime or Skype, when used in good faith for any telehealth treatment or diagnostic purpose, regardless of whether the telehealth service is directly related to COVID-19.
- Protecting staff and visitors. Staff and visitors alike can become infected and spread COVID-19. Medical staff will self-monitor for symptoms and report their illness to workmates and personal contacts. Wellpath will identify replacement staff, as necessary. Wellpath strongly encourages all facilities to consider eliminating in-person visitation, as well as “weekender” and work release programs. Video visitation, if available, is an effective substitute during this time of social distancing. Discourage contact visits from family and friends for their health and the health of the confined. When they visit, Wellpath will perform mandatory verbal screening and temperature checks to prevent suspected infections from entering the facility. Consider the mental health of the incarcerated by vigorously communicating decisions and reasons.
On March 29, 2020, the president extended the national social distancing effort an additional two weeks (through April 30), asking citizens to continue reducing contact with others to slow the upward curve of new infections and deaths – to stabilize and “flatten the curve.” Failure to do so could result in millions of infections and up to 200,000 deaths in America.
Wellpath stands with you to make the right decisions on the health of your facility – both staff and residents. Work closely with your Health Services Administrator or Regional Operations Director to follow CDC guidelines based on your unique requirements.